Cancer and the anti-cancer treatments prescribed by oncologists have long been known to have significant effects on muscle, causing a catabolic muscle wasting state and resulting in widespread and progressive atrophy of most muscle groups.1 This process contributes significantly to the cancer cachexia seen in up to 80 % of all patients with cancer, resulting in progressive weight loss, loss of muscle mass and decline in functional abilities.2 Cardiac atrophy describes the reduction in myocardial mass caused by a combination of a reduction in cell size and decreased cell numbers because of cell death. There is growing evidence that cancer and anti-cancer treatments cause cardiac atrophy,3 which results in impairment of the systolic and diastolic function of the heart. This impairment significantly adds to the burden of symptoms in such patients, including breathlessness, lethargy, reduced exercise tolerance and – on occasion – overt congestive cardiac failure as well as increased mortality.4 Improvements in cancer treatment and resulting survivorship have led to cardiovascular health in cancer patients becoming increasingly important. In one large registry of breast cancer patients, cardiovascular causes of death overtook breast cancer as the leading cause of death at nine years following the cancer diagnosis.5 As cardiologists and oncologists work together to explore models of care to improve outcomes for cancer patients, there is increasing understanding the functional changes to the heart resulting from both the cancer itself and various cancer therapies.
Cardiac Atrophy Induced by Cancer
As early as 1968, Burch et al. recognised that patients who died from malignancy had a heart mass smaller than average at post mortem.6 Histological analysis revealed a reduction in the size and number of cardiac muscle fibres and increased extracellular stroma surrounding the myocytes. More recently post-mortem studies by Springer et al. in patients who died of pancreatic, lung and colorectal cancer found extensive loss of cardiomyocyte volume and replacement with fibrotic tissue in all cancer patients.7 A subset of these patients who had experienced significant cancer-related weight loss and cachexia were noted to have reduced left ventricular (LV) wall thickness and total heart weight compared with cancer patients without cachexia. This finding suggests that cardiac atrophy in cancer is part of a complex, systemic metabolic syndrome caused by the cancer that results in widespread muscle wasting, including the myocardium.
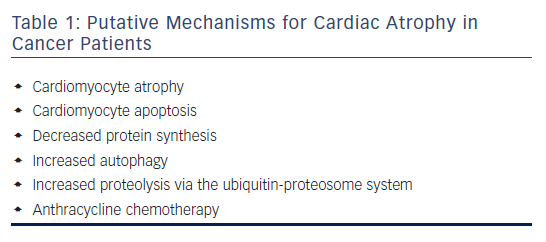
Rodent models of cancer cachexia also show characteristics of cardiac atrophy, including decreased heart weight and LV mass, the thinning of septal, interventricular and posterior walls and chamber dilation as shown by echocardiography.8–11 Cardiac atrophy in cancer cachexia is likely to be driven more by cellular atrophy than cell death by apoptosis,8,9 and the imbalance between protein degradation and protein synthesis is the major cause of cardiac atrophy in cancer cachexia.3 Heart size decreases when the protein degradation rate exceeds the protein synthesis rate, which is likely to be because of a combination of decreased protein synthesis,9 increased autophagy8–10 and increased proteolysis via the ubiquitin-proteosome system (UPS).11,12 The putative mechanisms for cardiac atrophy in cancer patient are summarised in Table 1.
Significant reduction in cardiac myofibrillar protein synthesis rate has been demonstrated in cachectic ApcMin/+ mice – a colorectal cancer model – via the suppression of the mechanistic target of rapamycin pathway.13 This reduction in myofibrillar protein levels in atrophic hearts has also been replicated in other studies.8,9,11 Increased autophagy in cardiac atrophy has been demonstrated by the upregulation of biomarkers beclin-1, p62 and LC3B in various rodent models.8–10 Cosper et al.8 also observed abundant autophagic vacuoles in atrophic hearts using electron microscopy. Musolino et al.10 showed that megestrol acetate treatment can improve cardiac function in cachectic rats by downregulating autophagy, revealing the contribution of autophagy to cardiac atrophy. The role of UPS in the pathogenesis of cardiac atrophy is unclear. Two studies have reported the induction of the E3 ubiquitin ligases muscle RING finger-1, atrogin-1 and muscle atrophy F-box in colon-26 tumour-bearing mice11 and murine adenocarcinoma of the colon 16-inoculated mice.12 The authors suggested that UPS is upregulated by pro-inflammatory cytokine interleukin-6 via the P44/42 mitogen-activated protein kinase (MAPK) pathway,11 or high levels of oxidative stress in the heart.12 However, other studies8,9 found no changes in protein ubiquitination in atrophic hearts compared with controls. The discrepancies among the studies could be a result of differences in cancer models, time points in the progression of cardiac atrophy and the dynamic nature of the UPS.
Cardiac Atrophy Induced by Cancer Treatments
In addition to the direct effects of malignancy on the health of the myocardium, a number of chemotherapeutic agents – in particular anthracyclines – have been associated with the development of heart failure in cancer survivors.4 Doxorubicin is associated with dosedependent cardiotoxicity, which limits its clinical use and efficacy as a chemotherapy treatment.14 Rodent models of doxorubicin-induced cardiomyopathy have shown significant reduction in heart weight,15–17 and the thinning of septal and LV posterior wall.13 This suggests that doxorubicin-induced cardiomyopathy sometimes involves cardiac atrophy. However, other doxorubicin-induced cardiotoxicity models have demonstrated cardiomyocyte hypertrophy, suggesting the response to doxorubicin varies depending on conditions and genetic predisposition, rather than representing a single pathological entity.15
Direct measurement of heart mass is not possible in the clinical setting. Non-invasive estimates of LV mass can be calculated most accurately using cardiac magnetic resonance imaging (cMRI). In patients presenting with anthracycline-associated cardiomyopathy there is a dose-related reduction in LV mass in keeping with atrophic changes in the myocardium.18 Similarly, cMRI measures of extracellular volume are higher in asymptomatic patients three years after treatment with anthracyclines. This supports the observation that reduction in cardiomyocyte density and increased fibrotic change appears before the onset of cardiac dysfunction or heart failure symptoms in cancer patients treated with anthracycline chemotherapy.19
Doxorubicin induces cell death in cardiomyocytes, which contributes directly to cardiac atrophy as the turnover of adult cardiomyocytes is too limited to replace cell loss.20 The molecular mechanisms of doxorubicin-induced cardiotoxicity are not fully understood. Proposed mechanisms include reactive oxygen species (ROS) generation and oxidative stress, topoisomerase-IIb (Top2b) inhibition and mitochondrial damage. The most widely accepted mechanism is the generation of excessive ROS by redox cycling between quinone and semiquinone forms of doxorubicin.21 ROS accumulation brings deleterious effects such as lipid peroxidation, destruction of mitochondrial membranes and DNA damage.22 Zhang et al. demonstrated the crucial role of Top2b using a mouse model with cardiomyocyte-specific deletion of Top2b that was protected against doxorubicin-induced cardiotoxicity.23
Damage to mitochondrial structure and function are one of the early cardiotoxic effects of doxorubicin observed in both animal and cell models.15,16,24 Mitochondrial dysfunction and damage contribute to cardiac atrophy as mitochondrial content and function are important mediators of muscle size.3 In cardiomyocytes, doxorubicin binds irreversibly to cardiolipin in the inner mitochondrial membrane, therefore concentrating doxorubicin in the mitochondria.25 Mitochondriatargeted antioxidants are shown to attenuate cardiotoxic effects of doxorubicin in rats,13,26 revealing the importance of mitochondrial ROS in doxorubicin-induced cardiotoxicity
Like cancer cachexia, doxorubicin can induce cellular atrophy in cardiomyocytes by disrupting the balance of protein synthesis and degradation. Doxorubicin induces protein ubiquitination27 and activates ubiquitin ligase atrogin-1 in cardiomyocytes both in vitro and in vivo via the p38-MAPK pathway.17 Wang et al. demonstrated that doxorubicin induces autophagy in mouse hearts, which in turn increases apoptosis and decreases cardiomyocyte size.28 Min et al. demonstrated that doxorubicin activates calpain in cardiac muscles in vivo.13 Active calpain can degrade over 100 cellular proteins including key sarcomeric proteins.29 The calpain specific inhibitor SJA attenuates doxorubicininduced cardiac wall thinning as well as reducing caspase-3 activation and apoptosis.13
Clinical Observations
Cardiac dysfunction is the physiological consequence of the molecular changes of cardiac atrophy and fibrosis. A reduction in the quantity and quality of contractile cells will cause deterioration in systolic function, and as cardiomyocytes are replaced by fibrotic tissue the diastolic relaxation of the heart deteriorates. Ideally identifying patients who have atrophic changes in the heart prior to the onset of cardiac dysfunction could enable earlier treatment and should improve outcomes.30 However, detecting myocardial damage prior to the onset of dysfunction is challenging.
Endomyocardial biopsy and histological biopsy scoring allows direct quantification of the degree of cardiomyocyte damage and cardiac atrophy. This correlates well with the development of cardiac dysfunction as measured by invasive cardiac haemodynamics, and appears prior to functional deterioration when measured by echocardiogram.31 However, this is an invasive test with significant risks and is not justifiable or practical to perform as a screening test in asymptomatic patients.
Currently, measurement of LV ejection fraction (LVEF) by 2D echocardiography is the most widely available and practical tool to monitor deterioration in cardiac function following cancer.32 Its usefulness is limited by poor reproducibility and accuracy; moreover, deterioration in ejection fraction represents a late change in the development of cancer-induced cardiomyopathy.33 This deterioration in function only occurs after significant cellular damage and death has already occurred.31
Techniques to improve the sensitivity of echocardiography have been used including LVEF by 3D echocardiography, dobutamine stress echo and global longitudinal strain by 2D echocardiography. All of these methods have been shown to be more sensitive at detecting deterioration in cardiac function in patients following cancer.33–35 However they all suffer from the same disadvantage: they are measuring a late feature of cardiomyocyte damage and cell death.
cMRI has several benefits over echocardiography. It provides the most accurate and reproducible measure of LVEF36 therefore allowing earlier and more reliable detection of a deterioration in cardiac function. It also allows measurement of several structural changes which precede functional changes. In particular measurement of T1-weighted early gadolinium signal enhancement in the myocardium and comparison with skeletal muscle signal intensity 3 days after anthracycline therapy predicts deterioration in LVEF at both 3 and 6 months.37 Measurement of myocardial oedema with T2-weighted imaging has also been shown in rodent and preliminary human studies to predict subsequent deterioration in LVEF following anthracycline treatment.38 As yet these methods are not in common clinical use, but trials are ongoing to confirm the ability of these methods to predict the diagnosis of anthracycline-mediated cardiotoxicity and expedite treatment of affected individuals.
Several studies have measured cardiac biomarkers in cancer patients receiving chemotherapy. Detection of rises in cardiac troponin during and after anthracycline-containing chemotherapy predicted future reduction in LVEF and clinical cardiac events.39 A similar study utilising contemporary higher sensitivity troponin assays also detected rises in breast cancer patients receiving anthracycline and human epidermal growth factor receptor 2-targeted therapies, and combined with measurement of the inflammatory biomarker myeloperoxidase, the increase in troponin predicted future decline in left ventricular function.40 These troponin rises during cardiotoxic chemotherapy are an indicator of cardiac injury, but it is not clear if they specifically relate to cardiac atrophy. A recent report measured cardiac biomarkers in patients at diagnosis of a new malignancy, prior to cancer treatment. Elevated troponin or natriuretic peptide levels in the blood of treatment-naïve cancer patients predicted all-cause mortality.41 This may relate to cardiac stress secondary to the underlying malignancy, with cardiac atrophy one of the potential contributing factors.
Clinical Treatment Strategies
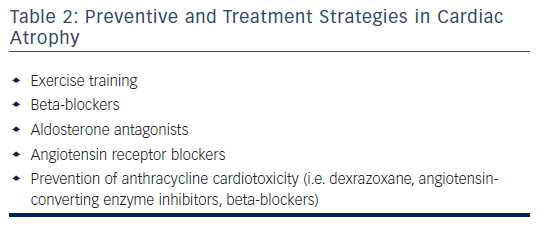
Treatment of cardiac atrophy caused by cancer and chemotherapy is challenging, and the development of cardiac dysfunction has been associated with a poor prognosis.30 However, recent studies using conventional heart failure treatment have begun to show benefits in this setting and the importance of early initiation of treatment appears even more pertinent in this group of patients.30Table 2 provides a summary of preventive and treatment strategies in cardiac atrophy.
Beta-blockers are a mainstay of systolic heart failure treatments and there is evidence supporting their use in cancer-induced cardiac atrophy. Beta-blockers have been shown to improve both symptoms and LVEF in humans; in rats they also increase total heart mass and reduce the overall body weight loss suggesting they have effects on the more generalised cachexia process.7,42 Beta-blockers represent a range of different molecular entities, and some appear to possess more apoptotic properties than others. For example, carvedilol has specific anti-apoptotic and antioxidant properties independent of its actions on beta-adrenergic receptors.
Similarly, aldosterone levels are significantly raised in cancer patients and the detrimental effects of mineralocorticoids on the myocardium are well studied.43 Treatment with the mineralocorticoid receptor antagonist spironolactone has been shown in a mouse model to reduce the level of fibrosis, reduce apoptotic cell death and improve markers of myocardial function.7
The role of angiotensin-converting-enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in cancer-related cardiac atrophy is less clear. In pre-clinical models ACE-inhibitors have failed to prevent loss of cardiac mass or improved markers of cardiac function and in some studies have exacerbated the loss of cardiac mass.3 Interestingly, losartan has shown more promise at improving LV mass and function and this raises the possibility that angiotensin-1 receptor activation may increase atrophy via transforming growth factor-beta signalling, and ARBs may have a specific protective effect in preventing cardiac atrophy.3
Perhaps the most clinically applicable and interesting is the role of exercise training to treat cancer cachexia as it promotes muscle development and improves cardiovascular fitness, and may have beneficial effects on cancer mortality. It is therefore likely to also be beneficial in cardiac atrophy, although at present evidence to support this is limited.44
There have also been attempts to prevent doxorubicin-induced cardiomyopathy by co-administration with the iron chelator dexrazoxane. Current understanding is that dexrazoxane reduces the production of iron-mediated ROS produced by doxorubicin, although it may also block doxorubicin binding to cardiac topoisomerase II-beta. Dexrazoxane has shown promising results to date in preventing future heart failure in paediatric oncology patients, and adults with metastatic breast and lung cancer by preventing a reduction in LVEF and reducing the incidence of symptomatic heart failure.45 The use of this has been limited by concerns about myelosuppression and a detrimental effect on the anticancer properties of doxorubicin, but further studies are ongoing to clarify its safety profile.46
Preventative treatment with carvedilol and enalapril in patients being treated for haematological malignancies was shown to have a small but statistically significant effect on preserving LVEF in the Prevention Of Left Ventricular Dysfunction With Enalapril And Carvedilol In Patients Submitted To Intensive Chemotherapy For The Treatment Of Malignant Hemopathies (OVERCOME) trial.47 Carvedilol monotherapy has also been shown to protect systolic and diastolic function when pre-emptively co-administered with anthracyclines48 and similarly spironolactone prevents deterioration in ejection fraction in patients treated with anthracyclines for breast cancer.49 These studies have relatively short follow-up duration and the longer-term outcomes of this approach remain unclear. Further studies are required before co-administration of heart failure treatments with anthracycline chemotherapy becomes routine practice.
Conclusion
The potential mechanisms underlying cardiac atrophy in cancer are complex, multifactorial and incompletely understood. Both cancer itself and chemotherapy may contribute to cardiac atrophy through a multitude of pathways, including disrupting the balance of protein metabolism and inducing cell death via ROS and mitochondrial damage. Understanding the mechanisms involved in driving cardiac atrophy can aid early identification of patients who are high risk or in the early stages of developing cardiac dysfunction. Further research in this area will focus on understanding the molecular pathways, developing more sensitive imaging modalities to facilitate early detection in patients and the development of targeted treatments which hopefully will have a beneficial impact on clinical outcomes including symptoms and mortality.