Hospitalisation is a critical event in the clinical course of heart failure (HF) and despite relatively rapid relief of symptoms, hospitalisation is followed by an increased risk of death and re-hospitalisation.1 While performance measures have been developed in the last few years with the intent of improving post-discharge outcomes, post-discharge mortality rates remain unchanged or have slightly worsened.2 The mechanisms of these high post-discharge event rates are incompletely understood3 and, to date, no treatment has improved such outcomes. Although long-term mortality is the result of the continuous deterioration of cardiac substrate, worsening of comorbidities, and progression of HF, there is considerable diversity of both the underlying pathophysiology and the patients involved, which makes it difficult to find an explanation that is suitable for all patients.4
Registry data reveal that 20 % of patients are discharged despite persistent signs and symptoms of HF, including minimal decrease or even increase in body weight. These findings suggest failure to relieve clinical congestion during the index hospitalisation may potentially contribute to the high post-discharge mortality rate.4
Post-hoc analyses of these clinical trials and international registries have identified several prognostic factors in AHF patients and have attempted to explore their relationship with post-discharge mortality. Knowledge of mortality predictors can be used to generate predictive models that can aid clinicians in their decision-making, in particular by identifying patients who are at high or low risk of death. These models could be used as a framework to discuss prognosis and provide evidence to support rational decision-making.
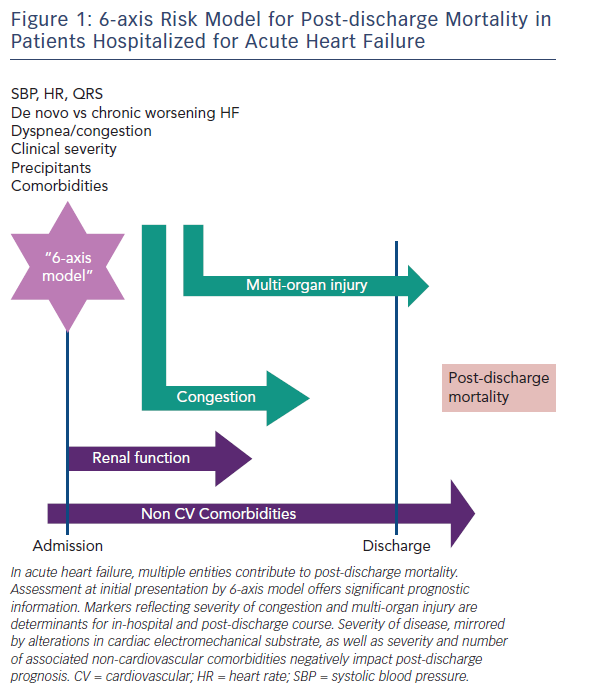
Even if the phenotypic heterogeneity of AHF patients5 makes it difficult to find a risk model suitable for all patients, many parameters are common to several of the models. Demographic characteristics, renal function, markers of organ injury, and non-cardiac comorbidities are included in most risk models (see Figure 1). Our goal in the present paper is to review the most important prediction models developed for the risk-stratification of patients with AHF.
Risk Stratification in Acute Heart Failure
Heart failure hospitalisation represents an important opportunity to assess patient prognosis. In the care of patients with HF, estimating and communicating prognosis is recommended by clinical guidelines6 and is considered to be an important component of high-quality health care. A better understanding of the mechanisms underlying the poor prognosis of patients hospitalised for HF may help provide better care and improve post-discharge mortality.
One of the major goals of AHF risk stratification is to match the risk profile of the patient with the type and intensity of care. AHF is not one distinct pathophysiologic entity, but rather a heterogeneous syndrome with multiple contributors to the progression of the disease and prognosis. A comprehensive assessment in these patients is necessary to identify multiple prognostic characteristics that may become possible therapeutic targets. Moreover, the phenotypic heterogeneity of AHF patients, either at presentation or during the hospital course, suggests that an algorithm is needed to classify these patients. For initial presentation, a “6-axis model” has been proposed to classify AHF patients.7 While this was designed for the initial assessment, each component of this model has long-term prognostic value (see Figure 1).
Candidate predictors can be obtained from patient demographics, clinical history, physical examination, disease characteristics, laboratory tests, and previous treatment. Studied predictors should be clearly defined, standardised, and reproducible to enhance generalisability and application of study results to practice.8 Prognostic studies use a multivariable approach in their design and analysis to determine the important predictors of the studied outcomes and to provide outcome probabilities for different combinations of predictors. The aim is to determine whether an outcome can reliably be attributed to a particular risk factor, with adjustment for other causal factors (confounders) using a multivariable approach.
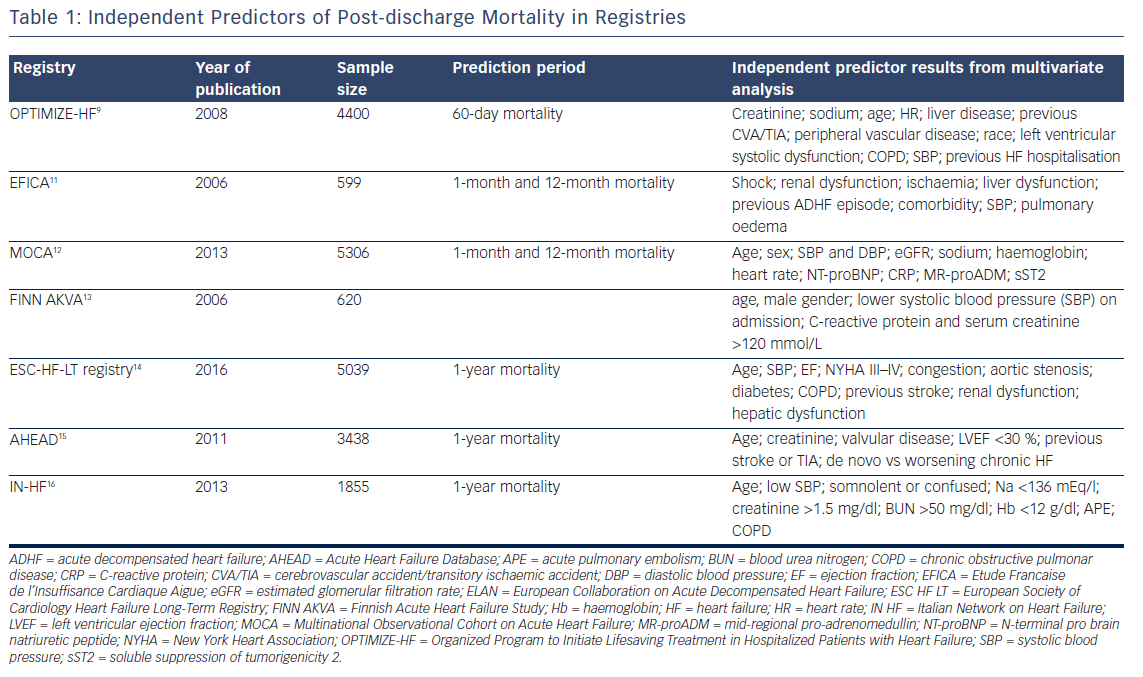
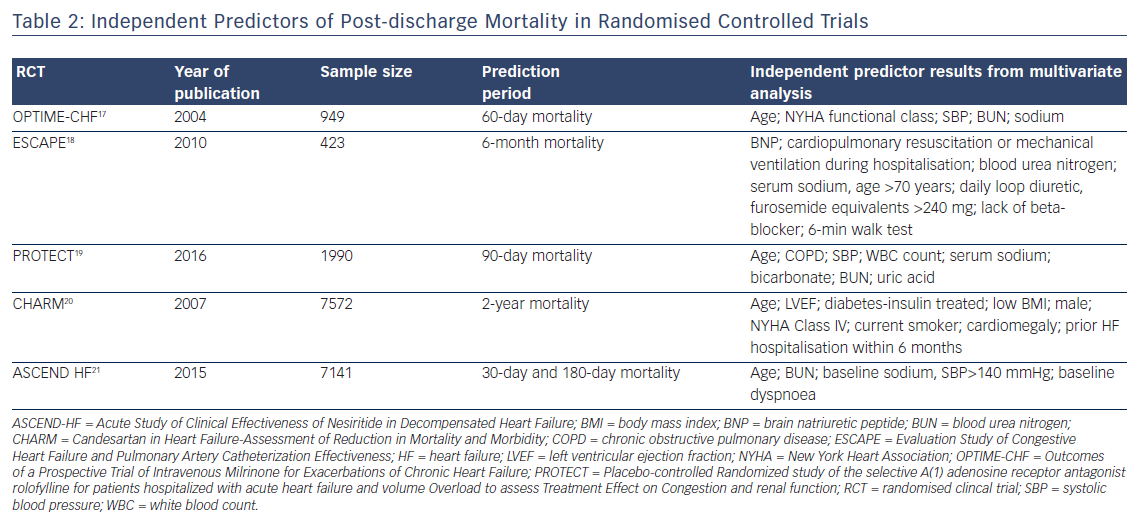
Predictors can be derived from registries (see Table 1) or from randomised clinical trials (RCTs) (see Table 2). Clinical characteristics of patients enrolled in RCTs may differ to those in the general population with HF, and prognostic models obtained from RCT data may have restricted generalisability because of strict eligibility criteria for the trial, low recruitment levels, lower rate of associated comorbidities, or large numbers of patients refusing consent. Registries have increased predictive power due to the large number of patients enrolled, but collection of clinical variables may not be as rigorous and complete as in RCTs.
One important consideration when assessing predictors of post-discharge mortality is the time frame of data collection.22 Variables collected upon admission may be less likely to be linked to 6-month or 1-year prognosis, as changes in clinical status or medical interventions performed during hospitalisation may affect medium or long-term outcomes. However, some variables collected at AHF admission are unmodifiable risk factors, such as age, gender and presence of comorbidities.
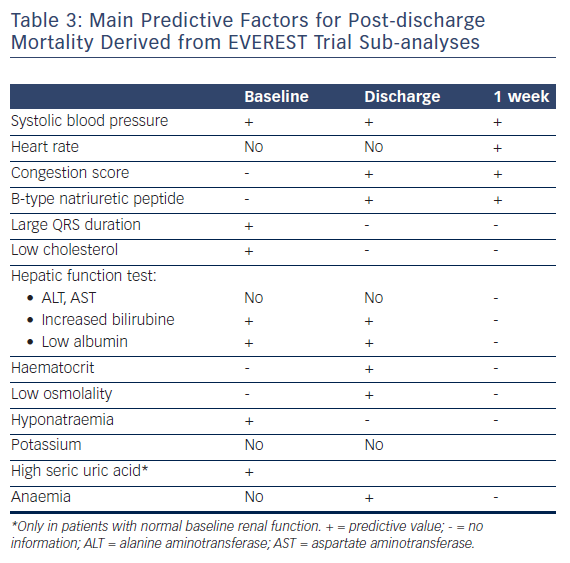
In addition, when considering all prognostic factors, it is important to carefully review the selection criteria for the cohort from which the predictor was reported. For example, some RCT enrolled patients with reduced ejection fraction (EF), while other RCTs were inclusive AHF irrespective of EF. Among patients with reduced EF, the Efficacy of Vasopressin Antagonism in Heart Failure: Outcome Study with Tolvaptan (EVEREST) trial database23 allowed the opportunity for numerous sub-analyses which have provided valuable insights in understanding post-discharge mortality predictors (see Table 3).
Variables Predictive of Post-discharge Outcomes in AHF
In RCTs and registries, the predictive factors for post-discharge mortality included age, history of previous hospitalisation, congestion, systolic blood pressure (SBP), heart rate (HR), QRS duration, renal function, markers of organ injury, and non-cardiac comorbidities (such as diabetes, cerebrovascular disease, chronic obstructive pulmonary disease, liver cirrhosis, and anaemia) (see Tables 1 –3). Although, there are many candidates that have additional prognostic value, the key variables are SBP and renal function. These two are the best discriminators between patients who survive hospitalisation and those who die or are readmitted post-discharge.
We have highlighted some of these important prognostic markers that are relevant in clinical practice.
Congestion
Clinical trials testing short-term IV therapies have focused on dyspnoea improvement. However, dyspnoea assessments remain imprecise and regardless of how it is measured, the vast majority of resolves or significantly improves in the first 24 to 48 hours of IV standard therapies.24 In the Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure (ASCEND-HF),25 the relationship between in-hospital dyspnoea improvement and post-discharge outcomes was inconsistent and study medication failed to show any post-discharge outcomes benefit. Furthermore, pathophysiology of congestion is more complex, and the subjective feeling of dyspnoea may poorly correlate with objective measures of decongestion, such as weight change25 or urine output.26
Nonetheless, congestion is the leading cause for AHF readmission, and represents an important therapeutic target of inpatient management, and a major determinant of discharge decision-making. Indeed, a clinical score, including orthopnoea, JVD and pedal oedema was used in the EVEREST trial, and this congestion score was associated with an increased risk of 30-day and 1-year mortality.27 However, despite the clinical importance of targeting signs and symptoms during hospitalisation, patients with absent or minimal signs and symptoms of congestion may experience a lower, but comparable, post-discharge event rate as compared to the overall cohort. This finding raises the hypothesis that treating beyond resolution of congestion may mediate improvements in post-discharge outcomes.7 Further research is necessary to prospectively validate the clinical utility of targeting provocative manoeuvres, including an assessment of orthopnoea, orthostatic hypotension, lung ultrasound, and completion of a 6-minute walk test and haemodynamic biomarkers, such as BNP/NT-proBNP, in patients hospitalized for HF.27
Natriuretic Peptides
Natriuretic peptides (NPs) represent a sensitive and noninvasive measure of ventricular filling pressures, which correlates with overall cardiac function and informs prognosis, irrespective of ejection fraction.28 During hospitalisation and the post-discharge period, persistence of elevated levels of NPs after resolution of clinical congestion signifies haemodynamic congestion.
In clinical studies, the absolute level of NPs measured at discharge29,30 and NPs percentage variation during hospitalisation31 correlate with post-discharge mortality. Also, BNP level at 1-week post-discharge was associated with the largest increase in prognostic value having the best accuracy of grading patients’ likelihood of death.32 Additionally, change in natriuretic peptide levels at hospitalisation to 1-month post-discharge carries incremental predictive value above the absolute value of the 1-month measurement alone.33
Systolic Blood Pressure
A large number of registries and RCTs have shown that systolic blood pressure (SBP) assessment at admission provides important, independent prognostic information in patients with HF with both reduced and preserved EF. Furthermore, SBP at hospital admission can effectively identify groups of patients that differ with respect to clinical characteristics, prognosis, underlying pathophysiology and therapeutic approach.34
In the EVEREST trial, low SBP determined either after the initiation of standard therapy or after the resolution of the “acute” phase of hospitalisation remained an indicator of poor prognosis.35
Elevated SBP in the acute setting is a result of high sympathetic tone, termed reactive hypertension, indicating the presence of functional cardiac reserve in the face of an acute physiologic stressor. In contrast, low, or even normal SBP at presentation, which may be the goal of treatment in the ambulatory setting, may be a more ominous finding, reflecting a low cardiac output and suboptimal or inadequate end-organ perfusion.34
Heart Rate
At the time of admission for AHF, heart rate (HR) is a reflection of the patient’s haemodynamic status,36 and changes in HR during hospitalisation have not been associated to short-term outcomes.37
A higher HR at both 1 and 4 weeks post-discharge was independently predictive of increased mortality during subsequent follow-up in patients with reduced EF and worsening HF.38
QRS Duration
Electrical dys-synchrony, as evidenced by a prolonged QRS duration, remains the currently accepted guidelines indicator to evaluate potential candidates for CRT.6 Prolonged QRS duration was independently associated with high post-discharge mortality in the EVEREST trial.39 The presence of a prolonged QRS duration associated with reduced LVEF is not only a marker for significantly increased mortality but becomes a potential therapeutic target. The Cardiac Resynchronisation in Heart Failure (CARE-HF) study demonstrated that CRT improved symptoms and reduced the risk of death in patients with reduced ejection fraction and prolonged QRS duration in the outpatient setting.40
Hyponatremia
In the ESC-HF-LT registry,41 hyponatremia (serum sodium <135 mEq/l) has been reported on admission at 25 % of patients and at discharge at 18 % of patients.
The pathophysiology of hyponatremia in HF has been described as a result of neurohormonal activation, including stimulation of vasopressin, which in complex interactions impairs water excretion (i.e. dilutional hyponatremia).42
Also, diuretic agents and several other common non-cardiac comorbidities may decrease serum sodium concentration.43 Hyponatremia is one of the most constant cited predictors of mortality in clinical trials and registries, and has been associated with a three-fold increase in post-discharge mortality.44
A similar finding has been found for serum osmolality and lower discharge serum osmolality was predictive of post-discharge outcomes in a sub-analysis of the EVEREST study.45
Although Tolvaptan was successful in reducing hyponatremia and increasing serum osmolality, inducing weight and fluid loss, it has not been shown to improve clinical outcomes.23 This suggests that hyponatremia and serum osmolality, despite of markers of prognosis, are not targets for drug therapy.
Distinct to hyponatremia, baseline and in-hospital changes in potassium, although may significantly impact in-hospital care and may limit the implementation of evidence-based therapies, they are not associated with all-cause mortality.46
Renal function
The majority of registries and RCTs considered baseline renal impairment as a predictor of poor outcome in AHF.47 Markers of renal function included serum creatinine, BUN, and uric acid.
Baseline creatinine has not been consistently included in prognostic models and a major limitation of this biomarker is that creatinine is not only filtered but is also secreted by the kidney, and its production is dependent on muscle mass.48
Although serum blood urea nitrogen (BUN) is considered to be a less specific marker of renal function compared with serum creatinine, it varies independently of changes in creatinine in HF patients because of neurohormonal activation and enhanced tubular reabsorption. Thus, elevated serum BUN in AHF patients may reflect both altered intrinsic renal function and potentially reversible “vasomotor nephropathy” secondary to the haemodynamic and neurohormonal effects of destabilised HF,49 and its predictive value extends beyond hospitalisation. Prognostic utility of high serum uric acid (sUA) is limited, and sUA is predictive of post-discharge mortality only in patients with preserved admission renal function.50
Markers of Organ Injury
Injury or end-organ dysfunction, including myocardial damage, worsening renal function, and hepatic impairment, have been independently associated with mortality in AHF. Although many other organs (e.g. brain, lung, intestine, endothelium, vasculature) are exposed to injury during AHF episodes, organ-specific injury markers for these organs suitable for clinical practice are missing.51 While data support such markers as prognostic, clinical trial efforts to date with therapies designed to abort end-organ injury during episodes of AHF have been disappointing.
Troponin
An increase in plasma troponin levels is very common in patients hospitalised for HF. The percentage of patients with “elevated” troponin in AHF depends substantially on the severity of HF, the cut-point chosen, as well as the sensitivity of the assay employed.52 Furthermore, Troponin release in AHF is often persistent. In ASCEND-HF, at 30 days post-discharge, 62 % of patients had detectable values of troponin I and 28 % had elevated values >99 % of URL53
Although the exact mechanisms of myocardial injury in HF are uncertain, ischaemia, haemodynamic stress, oxidative stress, inflammation, altered calcium handling and impaired renal clearance have all been proposed as mechanisms of troponin elevation.54
Multiple studies have evaluated the association between baseline elevated circulating cTn and post-discharge mortality in various AHF settings. Despite variations in study design, patient populations, and assay characteristics, there has been a mostly consistent association between cTn elevation and worsened post-discharge outcomes.55–57 Thus, measurement of cTnI in patients hospitalised for AHF is warranted, given the desire to identify patients at high risk for adverse outcomes, as well as to identify patients in whom ischaemia appears to be a trigger of decompensation.6
Studies have varied in the type of troponin assay used (I or T), traditional or high sensitivity (hsTn), as well as the cut-off values used to define a positive test. In addition to baseline values and a rise in serum troponin levels during hospitalisation, an index of an event-related myocardial necrosis, is a powerful predictor of outcomes.53,58 In the Placebo-Controlled Randomized Study of the Selective Adenosine A1 Receptor Antagonist Rolofylline for Patients Hospitalized with Acute Decompensated Heart Failure and Volume Overload to Assess Treatment Effect on Congestion and Renal Function (PROTECT) study, positive troponin at baseline, and conversion during hospitalisation from negative to positive levels, were associated with worse outcomes at 60 days.59 In the Relaxin in Acute Heart Failure (RELAX-AHF) study, an increase in troponin during the hospital stay had an independent relation with 180 days mortality.60
Worsening Renal Function
A review of the wide body of literature suggests an inconsistent relationship between in-hospital worsening renal function (WRF) and post-discharge outcomes. Data suggest that the clinical context of WRF is essentially in determining its prognostic implication. For example, WRF in the setting of effective decongestion, as exemplified by haemoconcentration, has consistently been associated with favourable long-term prognosis. This is often referred to as “pseudo worsening renal function”.61 Importantly, longitudinal follow-up of these patients shows a strong tendency for renal function to return to baseline, suggesting that no permanent renal injury takes place despite a change in laboratory values. In contrast, WRF outside the context of active fluid removal may predict worse outcomes.62 Thus, in patients with AHF, serum creatinine changes during admission are associated with adverse outcome only in the presence of congestion. Persistence of congestion during hospitalisation is the most important prognostic factor and WRF has clinical significance only when occurring in patients with persistent fluid overload.63 A further decline in eGFR (especially if urinary output decreases or the clinical status of a patient simultaneously deteriorates) may represent true WRF, which is associated with substantially worse long-term outcomes and thus should be avoided.47 Furthermore, targeting improvement or preservation of renal function did not lead to an improved survival rate in the PROTECT trial.64
Liver Injury
Previous studies conducted in patients hospitalised for HF65–68 have found the association between transaminases and mortality to not be statistically significant after adjusting for natriuretic peptide concentrations66 or invasive haemodynamic measurements.67,68 However, in RELAX I, increases in serum transaminases (AST and ALT) were associated with increased 180-day all-cause mortality.60
Comorbidities
Two-thirds of readmissions within 30 days from a HF hospitalisation are for non-HF primary issues, regardless of EF. Comorbidities are highly prevalent in this population, and not only do they precipitate rehospitalisation, uncontrolled comorbidities worsen HF over time.69
In the ESC-HF-LT-registry,14 a number of non-cardiac comorbidities, including hepatic or renal dysfunction, previous stroke, diabetes and chronic obstructive pulmonary disease (COPD), were found to be independent predictors for 1-year mortality in patients hospitalised for HF with both preserved and reduced EF.
Although without a graded relationship between baseline glycaemia and outcomes, diabetic status has been found to be one of the most important predictors of 1-year all-cause mortality, independent of EF, eGFR and other comorbidities.70
Concurrent COPD independently predicts mortality in patients with reduced and preserved ejection fraction,71–73 and greater airflow obstruction is associated with worsening survival.74
In EVEREST, anaemia at discharge, but not admission, was independently associated with increased all-cause mortality.75 However, it is unclear whether anaemia is truly a prognostic marker or a mediator of risk. It has been postulated that anaemia is a marker of disease severity for HF, or that other factors associated with anaemia are responsible for the increased events. Multiple RCTs have investigated the impact of anaemia treatment on mortality, including the recent RED-HF trial,76 but have failed to demonstrate significant benefit.
Since the aetiology of anaemia in AHF is multifactorial, targeting anaemia in the broad population with AHF may not be a viable strategy until there is an improved understanding of how anaemia or different components of anaemia directly affect post-discharge outcomes.
Risk Scores
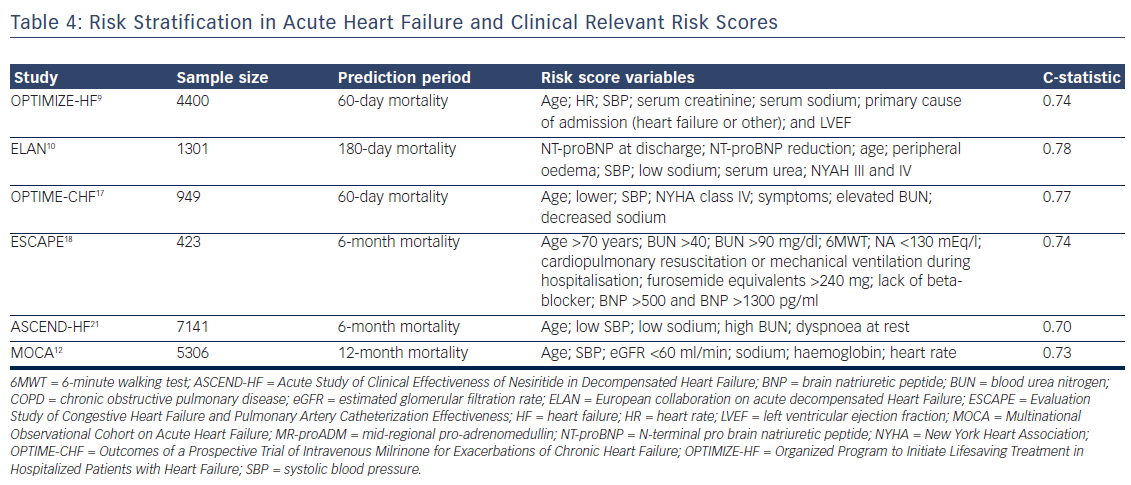
Post-hoc analyses have combined various risk markers from multi-variable models in risk scores, in order to better stratify patients and thus identify the highest-risk patients.23 Probability as an individual patient who experienced an event had a higher risk score than a patient who had not experienced the event is evaluated by C-statistic.77
Given the complexity and heterogeneity of AHF, prior attempts for risk modelling have not been easily adapted to clinical practice and generally have not had high discriminatory capacity. Most models were derived from demographic, clinical and biological data collected at admission (see Table 4) and only a few have used discharge data. Also, including a variable in a risk model will be negatively impacted by the quantity of missing data, and the rate of collection has varied among registries. Also, the current available models do not include the use of devices, which may carry a strong impact on prognosis in the long term.78 Actually, risk stratification by scoring methods remains only informative in the clinical decision-making process.
Limitation of Prognostic Models
Despite numerous clinical and biological variables showing in registries and RCTs independent predictive value for post-discharge mortality, very few represent true targets for in-hospital therapies such as congestion, QRS duration, and non-cardiac comorbidities. In addition, heart rate measured at 1-week and 1-month post-discharge could be considered a target for If antagonist Ivabradine. Although in the RELAX-AHF I trial markers of organ injury were associated with 180 days mortality and decreased as result of Serelaxin treatment, the RELAX II study did not confirm these beneficial effects.
Another major limitation of prognostic models in AHF is the absence of prospective validation and lack of the impact studies.
The main ways to evaluate or validate the performance of a prognostic model on a new dataset are to compare observed and predicted event rates for groups of patients (calibration) and to quantify the model’s ability to distinguish between patients who do or do not experience the event of interest (discrimination).77
Furthermore, studies to evaluate the effect of using a prognostic model on current medical practice and on patient outcome would be informative and could lead to clinical implementation of such a model.79 An impact analysis can determine whether use of the model is better than usual care.80 This remains an unmet need.
Conclusion
In AHF, the attempts to develop risk models are justified by the evidence that the risk of post-discharge mortality and rehospitalisation remains high. Furthermore, developing risk models would aid in targeting limiting resources to the appropriate patients. Even if the phenotypic heterogeneity of AHF patients makes it difficult to find a risk model suitable for all patients, some parameters recur in many models. However, in spite of limitations, prognostic models add to our understanding of the determinants of the course and outcome of patients with AHF. The impact of stratification of AHF patients on current clinical practice should be further evaluated in prospective studies.
Acknowledgement
All of the authors acknowledge the important contribution of Professor Mihai Gheorghiade in this manuscript, which represents only one of his hundreds of research contributions. Mihai Gheorghiade was one of the most respected, quoted and liked cardiologists. Committed to excellence from early on in his career he was determined to excel in patient care, research and teaching. He felt that his highest calling was to mentor students, trainees, and junior colleagues. He was never more enthusiastic than when supporting new collaborations to take place between great minds in different countries. He passed away on 24 August 2017. The world of cardiology has lost an iconic figure, but his legacy of challenging concepts will live on for many years to come.